article
Real-Time Operational MDM: The Missing Link
SECTIONS
You have invested millions in Master Data Management (MDM). You have a Golden Record for your providers and members. So why is your provider directory still inaccurate? Why are claims still getting rejected due to "unknown provider" errors? And why, when a member calls to ask if their new specialist is in-network, does your service rep have to check three different screens to give a confident answer?
The uncomfortable truth is that for the last twenty years, healthcare has been buying storage solutions for a logistics problem.
Traditional MDM was built to create a snapshot—a clean, deduplicated record stored safely in a warehouse. But healthcare doesn't happen in a warehouse. It happens in real-time. It is a messy, dynamic web of relationships that change every second.
If your data strategy is focused on creating a static Source of Truth, you are already behind. It is time to stop building data museums and start building an Operational Health Data Management system.
The "Static Snapshot" Trap
Most health plans treat MDM as a periodic cleaning exercise. You ingest data from credentialing, claims, and roster files; you scrub it; you match it; and you store it.
The problem is the lag time. By the time that "clean" record makes it back to your operational systems, the reality on the ground has changed. A provider has moved. A network contract has expired. A patient has divorced and revoked consent.
As noted in Healthcare IT Today, legacy systems and static data strategies are "slowing progress, increasing costs, and limiting the ability to leverage real-time insights." When your MDM is disconnected from your daily transactions, your "Golden Record" is just a rusty snapshot of the past.
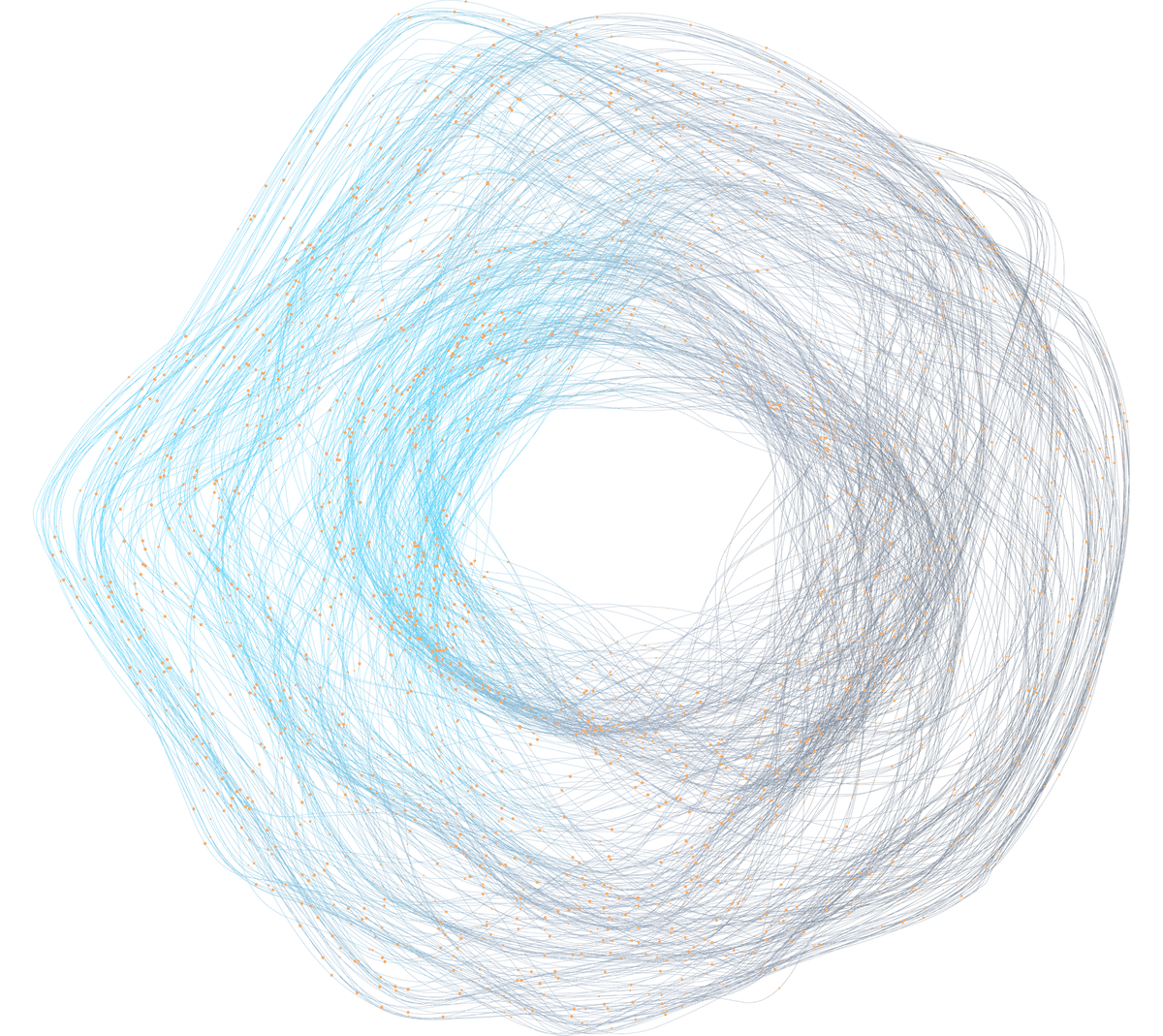
The Graph Reality: It’s Not a List, It’s a Web
One of the biggest educational hurdles in health data management is moving past the idea of rows and columns.
In reality, your data is a graph of interconnected entities. Consider the complexity of a single provider record:
- Dr. Deborah Johnson (Provider)
- Works at 742 Evergreen Terrace (Service Location)
- Which is part of Springfield Medical Group (Organization)
- Which contracts with Blue Advantage HMO (Network)
- Which is a product of HCSC (Payer)
If Dr. Johnson leaves Springfield Medical Group, it changes more than just her profile. It ripples through the entire chain. That location is no longer valid for her. That network affiliation might end. Any claims submitted for her at that location under that network need to be flagged immediately.
Traditional MDM struggles to traverse these "grandchildren" relationships. Gaine’s Health Data Management Platform (HDMP) uses a cross-domain model that understands these connections natively. It doesn't just master the provider; it masters the relationships between the provider, the location, the plan, and the patient.
The Shift: Transactional MDM
Here is the concept that might be new to you: Transactions should inform the Master.
In a typical setup, MDM is a downstream consumer. It waits for data to land. In an Operational Data Management model, the MDM is an active participant in the data flow.
Imagine a claim comes in for a provider who isn't in your master index yet. In the old world, this claim hits a suspense queue and sits there for days until a human reviews it.
In an operational model like Gaine HDMP, that transaction is processed in sub-second time. The platform analyzes the incoming claim data, compares it against external reference databases (like NPPES or DEA), and can tentatively build a profile for that provider on the fly. The transaction itself helps build the master record.
This shifts your data strategy from reactive cleanup to proactive intelligence.
AI That Actually Governs
We hear a lot about Generative AI writing emails or summarizing notes. But in data management, AI has a much more boring—and much more valuable—job: Deterministic Governance.
Governance shouldn't be a PDF of rules that no one reads. It should be a digital gatekeeper.
With Gaine HDMP, data health rules are fired the instant a new bit of data arrives.
- Example: A roster file comes in listing a provider’s birth year as 2015. A simple rule set—"Practicing provider must be between 22 and 90 years old"—catches this immediately.
- AI Context: Beyond simple rules, AI can analyze a profile against the entire population. It can tell a Data Steward, "This provider record has higher volatility than 90% of your network," flagging it for review before it corrupts your directory.
This allows you to move from finding errors next month to preventing errors in real time.
Unify, Control, Synchronize
To fix the data silos that HealthTech Magazine correctly identifies as impediments to care, you need a platform that does three things simultaneously:
- Unify: Bring Provider, Member, Payer, and Clinical data into one cross-domain model.
- Control: Apply governance rules in real-time to every transaction.
- Synchronize: Ensure that when a change happens in one place, it is propagated to every system that needs to know.
This is the promise of Gaine HDMP. It’s not just about better data; it’s about aligning your digital reality with the physical one.
Stop Managing Silos
Your members expect your app to work. Your providers expect to get paid. Your compliance team expects to pass audits. None of this happens if your data is stuck in a static warehouse.
It is time to embrace Operational Data Management. Let’s make your data as active and dynamic as the healthcare system it supports.
Ready to see what your data looks like when it’s alive? Explore Gaine HDMP today.

